Lis Copays 2020


 Below is a comparison of the Standard Benefit Model Plan parameters as released by The Centers for Medicare and Medicaid Services (CMS) for the plan years 2022 through 2006.
Below is a comparison of the Standard Benefit Model Plan parameters as released by The Centers for Medicare and Medicaid Services (CMS) for the plan years 2022 through 2006.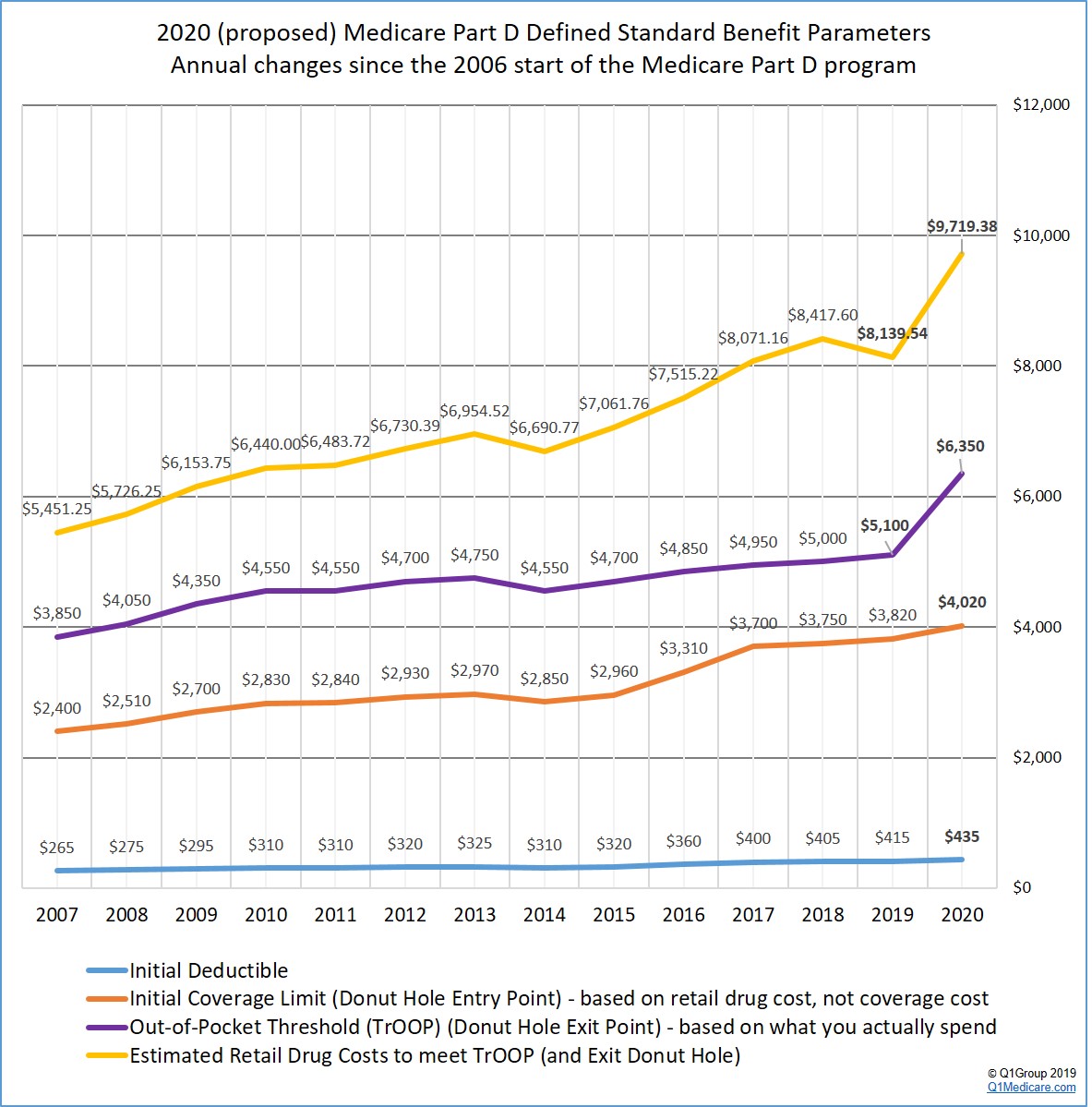
| Medicare Part D Benefit Parameters for Defined Standard Benefit 2006 through 2022 Comparison | |||||||||||||||||
| Part D Standard Benefit Design Parameters: | 2022 | 2021 | 2020 | 2019 | 2018 | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 | 2010 | 2009 | 2008 | 2007 | 2006 |
| Deductible - After the Deductible is met, Beneficiary pays 25% of covered costs up to total prescription costs meeting the Initial Coverage Limit. | $480 | $445 | $435 | $415 | $405 | $400 | $360 | $320 | $310 | $325 | $320 | $310 | $310 | $295 | $275 | $265 | $250 |
| Initial Coverage Limit - Coverage Gap (Donut Hole) begins at this point. (The Beneficiary pays 100% of their prescription costs up to the Out-of-Pocket Threshold) | $4,430 | $4,130 | $4,020 | $3,820 | $3,750 | $3,700 | $3,310 | $2,960 | $2,850 | $2,970 | $2,930 | $2,840 | $2,830 | $2,700 | $2,510 | $2,400 | $2,250 |
| Out-of-Pocket Threshold - This is the Total Out-of-Pocket Costs including the Donut Hole. | $7,050 | $6,550 | $6,350 | $5,100 | $5,000 | $4,950 | $4,850 | $4,700 | $4,550 | $4,750 | $4,700 | $4,550 | $4,550 | $4,350 | $4,050 | $3,850 | $3,600 |
| Total Covered Part D Drug Out-of-Pocket Spending including the Coverage Gap - Catastrophic Coverage starts after this point. See note (1) below. | $10,012.50 (1) | $9,313.75 (1) | $9,038.75 (1) | $7,653.75 (1) | $7,508.75 (1) | $7,425.00 (1) | $7,062.50 (1) | $6,680.00 (1) | $6,455.00 (1) | $6,733.75 (1) | $6,657.50 (1) | $6,447.50 (1) | $6,440.00 plus a $250 rebate | $6,153.75 | $5,726.25 | $5,451.25 | $5,100.00 |
| Total Estimated Covered Part D Drug Out-of-Pocket Spending including the Coverage Gap Discount (NON-LIS) See note (2). | $10,690.20 plus a 75% discount on all formulary drugs | $10,048.39 plus a 75% discount on all formulary drugs | $9,719.38 plus a 75% discount on all formulary drugs | $8,139.54 plus a 75% brand discount | $8,417.60 plus a 65% brand discount | $8,071.16 plus a 60% brand discount | $7,515.22 plus a 55% brand discount | $7,061.76 plus a 55% brand discount | $6,690.77 plus a 52.50% brand discount | $6,954.52 plus a 52.50% brand discount | $6,730.39 plus a 50% brand discount | $6,483.72 plus a 50% brand discount | |||||
| Catastrophic Coverage Benefit: | |||||||||||||||||
| Generic/Preferred Multi-Source Drug (3) | $3.95 (3) | $3.70 (3) | $3.60 (3) | $3.40 (3) | $3.35 (3) | $3.30 (3) | $2.95 (3) | $2.65 (3) | $2.55 (3) | $2.65 (3) | $2.60 (3) | $2.50 (3) | $2.50 (3) | $2.40 (3) | $2.25 (3) | $2.15 (3) | $2.00 (3) |
| Other Drugs (3) | $9.85 (3) | $9.20 (3) | $8.95 (3) | $8.50 (3) | $8.35 (3) | $8.25 (3) | $7.40 (3) | $6.60 (3) | $6.35 (3) | $6.60 (3) | $6.50 (3) | $6.30 (3) | $6.30 (3) | $6.00 (3) | $5.60 (3) | $5.35 (3) | $5.00 (3) |
| Part D Full Benefit Dual Eligible (FBDE) Parameters: | 2022 | 2021 | 2020 | 2019 | 2018 | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 | 2010 | 2009 | 2008 | 2007 | 2006 |
| • Deductible | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 |
| • Copayments for Institutionalized Beneficiaries | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 |
| Maximum Copayments for Non-Institutionalized Beneficiaries | |||||||||||||||||
| Up to or at 100% FPL: | |||||||||||||||||
| • Up to Out-of-Pocket Threshold | |||||||||||||||||
| - Generic / Preferred Multi-Source Drug | $1.35 | $1.30 | $1.30 | $1.25 | $1.25 | $1.20 | $1.20 | $1.20 | $1.20 | $1.15 | $1.10 | $1.10 | $1.10 | $1.10 | $1.05 | $1.00 | $1.00 |
| - Other Drugs | $4.00 | $4.00 | $3.90 | $3.80 | $3.70 | $3.70 | $3.60 | $3.60 | $3.60 | $3.50 | $3.30 | $3.30 | $3.30 | $3.20 | $3.10 | $3.10 | $3.00 |
| • Above Out-of-Pocket Threshold | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | |
| Over 100% FPL: | |||||||||||||||||
| • Up to Out-of-Pocket Threshold | |||||||||||||||||
| - Generic / Preferred Multi-Source Drug | $3.95 | $3.70 | $3.60 | $3.40 | $3.35 | $3.30 | $2.95 | $2.65 | $2.55 | $2.65 | $2.60 | $2.50 | $2.50 | $2.40 | $2.25 | $2.15 | $2.00 |
| - Other Drugs | $9.85 | $9.20 | $8.95 | $8.50 | $8.35 | $8.25 | $7.40 | $6.60 | $6.35 | $6.60 | $6.50 | $6.30 | $6.30 | $6.00 | $5.60 | $5.35 | $5.00 |
| • Above Out-of-Pocket Threshold | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 |
| Part D Full Subsidy - Non Full Benefit Dual Eligible Full Subsidy Parameters: | 2022 | 2021 | 2020 | 2019 | 2018 | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 | 2010 | 2009 | 2008 | 2007 | 2006 |
| Eligible for QMB/SLMB/QI, SSI or applied and income at or below 135% FPL and resources ≤ $9,470 (individuals in 2021) or ≤ $14,960 (couples, 2021) (4) | |||||||||||||||||
| • Deductible | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 |
| • Maximum Copayments up to Out-of-Pocket Threshold | |||||||||||||||||
| - Generic / Preferred Multi-Source Drug | $3.95 | $3.70 | $3.60 | $3.40 | $3.35 | $3.30 | $2.95 | $2.65 | $2.55 | $2.65 | $2.60 | $2.50 | $2.50 | $2.40 | $2.25 | $2.15 | $2.00 |
| - Other Drugs | $9.85 | $9.20 | $8.95 | $8.50 | $8.35 | $8.25 | $7.40 | $6.60 | $6.35 | $6.60 | $6.50 | $6.30 | $6.30 | $6.00 | $5.60 | $5.35 | $5.00 |
| • Maximum Copay above Out-of-Pocket Threshold | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 |
| Partial Subsidy Parameters: | 2022 | 2021 | 2020 | 2019 | 2018 | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 | 2010 | 2009 | 2008 | 2007 | 2006 |
| Applied and income below 150% FPL and resources between $14,790 (individual, 2021) or $29,520 (couples, 2021) (category code 4) (4) | |||||||||||||||||
| • Deductible | $99.00 | $92.00 | $89.00 | $85.00 | $83.00 | $82.00 | $74.00 | $66.00 | $63.00 | $66.00 | $65.00 | $63.00 | $63.00 | $60.00 | $56.00 | $53.00 | $50.00 |
| • Coinsurance up to Out-of-Pocket Threshold | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% | 15% |
| • Maximum Copayments above Out-of-Pocket Threshold | |||||||||||||||||
| - Generic / Preferred Multi-Source Drug | $3.95 | $3.70 | $3.60 | $3.40 | $3.35 | $3.30 | $2.95 | $2.65 | $2.55 | $2.65 | $2.60 | $2.50 | $2.50 | $2.40 | $2.25 | $2.15 | $2.00 |
| - Other Drugs | $9.85 | $9.20 | $8.95 | $8.50 | $8.35 | $8.25 | $7.40 | $6.60 | $6.35 | $6.60 | $6.50 | $6.30 | $6.30 | $6.00 | $5.60 | $5.35 | $5.00 |
| (1) Total Covered Part D Spending at Out-of-Pocket Threshold for Non-Applicable Beneficiaries - Beneficiaries who ARE entitled to an income-related subsidy under section 1860D-14(a) (LIS) | |||||||||||||||||
| (2) Total Covered Part D Spending at Out-of-Pocket Threshold for Applicable Beneficiaries - Beneficiaries who are NOT entitled to an income-related subsidy under section 1860D-14(a) (NON-LIS) and do receive the coverage gap discount. For 2022, the weighted gap coinsurance factor is 89.1745%. This is based on the 2020 PDEs (91.76% Brands & 8.24% Generics) | |||||||||||||||||
| (3) The Catastrophic Coverage is the greater of 5% or the values shown in the chart above. In 2022, beneficiaries will be charged $3.95 for those generic or preferred multisource drugs with a retail price under $79 and 5% for those with a retail price greater than $79. For brand-name drugs, beneficiaries would pay $9.85 for those drugs with a retail price under $197 and 5% for those with a retail price over $197. | |||||||||||||||||
| (4) This amount includes the $1,500 per person burial allowance. The resource limit may be updated during contract year 2022. | |||||||||||||||||
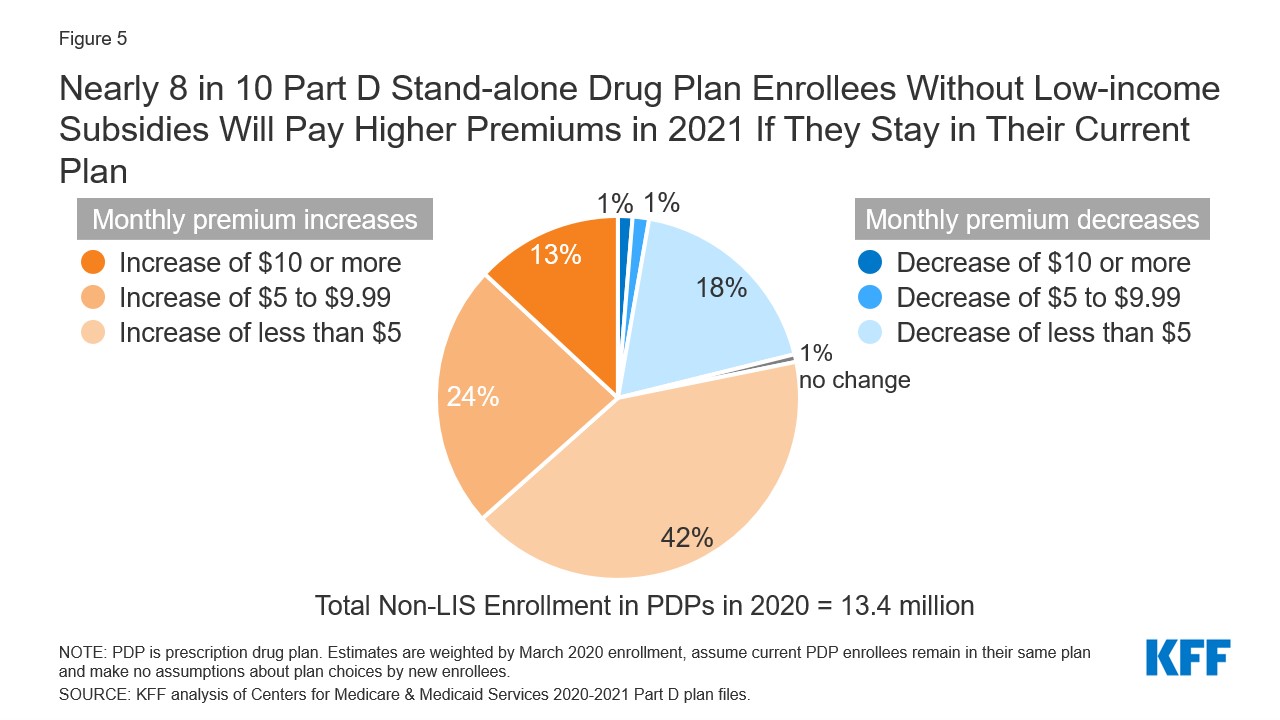
Amsterdam lies towards the bottom of Noord-Holland or North Holland, which is the northwestern-most province of Amsterdam.Suid-Holland, or South Holland, is approximately 20 miles (32 kilometers) southwest of Amsterdam, while the province of Utrecht—not considered Holland—is directly south of. Standard Copay Range3,a LIS Copay2 No more than $9.20b aBlue Cross Blue Shield of Michigan data are being used as an example. Other Part D carriers may have both lower or higher copay amounts. The estimated cost information is for a one-month supply of drugs from an in-network preferred pharmacy. No No Copay: $3.60 generic/$8.95 brand Catastrophic Copay: $0 Partial Low-Income Subsidy (LIS)/Extra Help (2020) - ALASKA Beneficiary Group Income Eligibility Requirement Monthly Income Eligibility Requirement Asset Eligibility Requirement Need to apply for LIS? Monthly Premium Annual Deductible Copay/Coinsurance Plan’s Formulary Drugs.
:max_bytes(150000):strip_icc()/medicare-part-d-costs-4589863_FINAL-a334073127ad461fbd5457a7d74d1e6c.png)
Lis Copays 2020 Form
Sign-up for our 2022 Reminder Service
Lis Copay Levels 2020
Cms Lis Copays 2020
Medicare Part D Benchmark 2020
